Acute renal failure
We say that we are facing acute renal failure when its onset is relatively early, less than three months. It can be reversible if it is treated in an appropriate and timely manner.
Chronic renal failure, acute exacerbation is the installation of acute renal failure in a patient with chronic renal failure.
Chronic renal failure
We say that we are facing chronic kidney failure ( CRF ) when it is possible to determine that kidney failure has existed for more than three months.
The name of this entity was changed to chronic kidney disease as there are situations of kidney disease/injury without failure. Examples of such situations are albuminuria/proteinuria, changes in urinary sediment, renal ultrasound changes, anatomopathological kidney lesions in renal biopsy or even a kidney transplant.
Stages of chronic renal failure
Chronic kidney disease has several stages or phases, causes, and degrees of albuminuria. The stages of chronic renal failure are as follows:
Stage 1 – Glomerular filtrate> = 90 -normal or elevated renal function;
Step 2 – glomerular filtrate 60-89 – decreased renal function with mild;
Stage 3a – Glomerular filtrate from 45 to 59 – renal function with mild to moderate decrease;
Stage 3b – Glomerular filtrate from 30 to 44 – renal function with moderate to severe decrease;
Stage 4 – Glomerular filtrate from 15 to 29 – renal function with severe decrease;
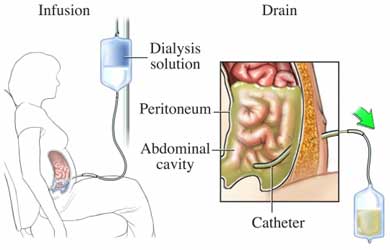
Stage 5 – Glomerular filtrate <15 -Renal failure (add D if the patient is on dialysis).
Glomerular filtrate values in (mL / min / 1.73 m2).
Pathophysiology of renal failure
The pathophysiology of renal failure, acute or chronic, can have different levels. If the pathology that damages the kidneys is found “before” the kidneys, it is called the renal failure of a pre-renal cause, as for example in cases associated with heart failure or the removal of volume in the vessels.
In turn, if the pathology is intrinsic to the kidneys, as is the case of acute glomerulonephritis or pyelonephritis, renal failure is considered to be of renal cause.
Finally, if the cause of renal failure is related to obstruction of urinary drainage, such as prostate hypertrophy, it is called post-renal.
Find out below what the symptoms of kidney failure are.
Symptoms in renal failure
The signs and symptoms of kidney failure are usually late, so they appear in the more advanced stages of chronic kidney disease. They can result from decreased glomerular filtration, such as edema (swelling), decreased urinary elimination or high blood pressure.
In stage 4, or more commonly in stage 5, more evident signs or symptoms may appear, such as generalized weakness (asthenia), lack of appetite (anorexia), nausea, vomiting, and changes in the central nervous system (slowness of reasoning, drowsiness) and rarely seizures).
These initial symptoms of chronic renal failure are explained to patients who are already being followed up with nephrologist in Delhi. In most cases, however, kidney disease is detected in routine tests without previous suspicion of its existence.
In India, cases of chronic renal failure that are diagnosed only at stage 5, using the emergency service to start hemodialysis on an emerging basis, have decreased. This improvement is mainly due to the improvement of primary health care with timely referral to kidney specialist in Delhi.
Causes of kidney failure
The causes of renal failure are multiple and vary according to the age group. As an illustrative example, the aetiology of chronic kidney diseases that led to the beginning of regular dialysis in Delhi: diabetes mellitus 33.9%, arterial hypertension 13.1%, glomerulonephritis chronic 11.2%, polycystosis 4.9%, hypoplasia / renal dysplasia 0.7%, other causes 18.5% and unknown causes 17.7%.
Children only reach “normal” kidney function at two years of age, so below that age, the classification of chronic kidney failure at the stages mentioned above cannot be applied.
The vast majority of cases of kidney failure in early stages are, in general, related to congenital kidney diseases. However, the causes of kidney failure in pediatrics, requiring dialysis or kidney transplantation, also include glomerular diseases.
Diagnosis of renal failure
The diagnosis of renal failure can be made by family doctors, taking into account some aspects, namely:
- The complete absence of diuresis (anuria) is not a characteristic of chronic renal failure, but of acute renal failure or acute chronic kidney failure;
- Elevated creatinine and serum urea are characteristic of renal failure;
- To better characterize the stage of chronic renal failure, creatinine clearance is used using 24-hour urine collection (determination of urinary volume and creatinine) and blood (determination of serum creatinine): creatinine clearance = urinary creatinine (mg / dl) / serum creatinine (mg / dl) X urine volume of 24 hours (ml) / 1440 (minutes). It is expressed in ml / minute (normal values: men> 90 ml / minute; women> 80 ml / minute). Formulas can also be used to calculate creatinine clearance, avoiding the 24-hour urine collection that is often not performed correctly or is not feasible;
- The signs and symptoms of chronic kidney disease should lead to an assessment of renal function (serum creatinine and urea, as well as creatinine clearance using mathematical formulas or with 24-hour urine collection as already described);
- Elevated serum potassium values are not essential for diagnosis;
- Other common analytical changes in chronic kidney disease in advanced stages (3 to 5) are anemia, metabolic acidosis, low serum calcium, and elevated parathormone;
- Summary analysis of urine may reveal albuminuria and urinary sediment may show changes such as hematuria and erythrocyte cylinders;
- Renal ultrasound is the exam indicated for initial imaging evaluation in suspected chronic kidney disease. It may reveal a decrease in kidney size, although in diabetes mellitus this change may not exist even in advanced stages of CRF. Another echographic abnormality typical of chronic kidney disease is the decrease in differentiation between the cortex and the renal medulla. If multiple bilateral renal cysts appear, we may be in the presence of a polycystic disease.
The early referral of patients with chronic renal failure to the best nephrologist in Delhi has had an impact on improving their follow-up, with implications for delaying their progression as well as for the adequate treatment of the various complications of chronic renal failure.
How to prevent kidney failure?
Renal failure can be prevented, essentially through the following measures:
- Lifestyle changes to prevent frequent causes of chronic renal failure, such as type 2 diabetes or cardiovascular disease including high blood pressure;
- Obesity (overweight) can also be associated with chronic kidney failure. Lifestyle should be changed in order to avoid obesity;
- Avoid exposure to nephrotoxic drugs, especially non-steroidal anti-inflammatory drugs.